Check out this fantastic compilation of information relating to back pain that is presented by Ben at Cor-Kinetic!
A great bit of free information to help people who have/are experiencing pain to learn and gain a little better understanding.
*IMPORTANT – This document does not replace professional medical advice and is only intended for information purposes.*

BACK PAIN INFORMATION
- Back pain is normal. Up to 20% of people are likely to get some each year and a whopping 80% of us will get some back pain in our lifetime, in fact it would abnormal not to get back pain.
• Back pain can last up to 6 weeks – this maybe longer than you anticipated. So if it has been going on for a bit there is no need to unduly worry. Lots of pains only last a number of days but it is still normal for it to last longer.
• Although we all know someone who has had long term persisting back pain that has caused lots of problems it is actually somewhere between 10% and 25% of people with back pain that lasts longer than normal. So you have good odds it won’t last longer than 6 weeks.
• Back pain is no different to any other pain in our bodies such as shoulder, ankle or knee pain although people do tend to worry more about it.
• Pain itself is normal and nothing to be scared of. It is a protective mechanism that has evolved help us out. You would not want to live without it!
• Pain is not a good at reflecting the physical state of our back or any body part. We can have lots of pain without significant damage. Think about getting a paper cut or a bee sting. They can hurt like hell but don’t really damage us.
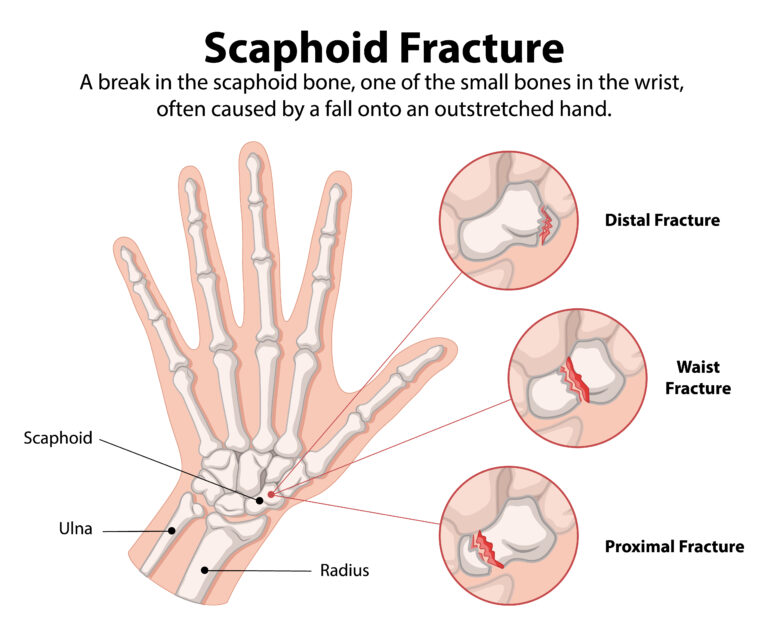
DIAGNOSIS
Diagnosis can often be challenging with back pain although I know that people often want an answer. We don’t always need a definitive answer to help you. Here is what we do know:
- The vast majority of back pain is not serious, in fact around 99%. The 1% is mostly fractures, can include cancer, but these a pretty rare occurrences.
- Around 10% can be pinned down to a specific tissue diagnosis such as a disc or a nerve.
- These statistics mean that it is unlikely to be a ‘slipped disc’ or a nerve problem and people often throw these terms around as causes without really knowing this for sure. This can often be unhelpful.
- Therapists have some tests to tell if the problem is in that 10%. These include clinical tests for the nerves and nerve roots as well as muscle strength, sensation and reflex tests.
- It is very difficult to make a diagnosis from a MRI alone. Lots of MRI findings also exist in people without pain, hence the need for a clinical exam to accompany a scan.
- MRI’s are not able to show us pain.
- We often can’t pin it down to a specific tissue or pathology around 9 out of 10 times. There are lots of different tissues in a small space and if it is irritated or inflamed then it may affect more than one of the tissues.
- Inflammation is a good thing. It means the body is working well and doing its repair jobs.
- From a medical perspective this type of back pain is often termed ‘non-specific’ and we should see this as a positive diagnosis as it means nothing serious is wrong. It could still hurt a whole lot though.
- The term ‘non-specific’ means the tissue, not non-specific to you or has no origin. YOUR PAIN IS ALWAYS REAL AND SPECIFIC.
- Non-specific pain often responds well to moving and although we cannot give an exact label does not mean we cannot give some ideas to help or an a basic explanation about why you might have back pain.
OTHER FACTORS
- Lots of different factors (many which you may have not considered) can affect your back pain.
• This can mean that you feel your back pain has a life of its own but it maybe that you have not been informed about or considered all of the potential contributing factors.
• These other factors can include abnormal sleep, lots of life stressors including work and family, feeling that the pain will never go and negative beliefs about your back and performing daily activities.
• Its probably not your spinal posture, your pelvic tilt, a teeny weeny muscle not firing or something needing to be put back into place causing your back pain. How do we know? We have studied this stuff to death.
• If you have been told this before it could mean your therapist is not up to date with the latest research in this area. You may have been given lots of opinions previously and it can often be confusing for you and hence the need to be aware of the scientific data in this area.
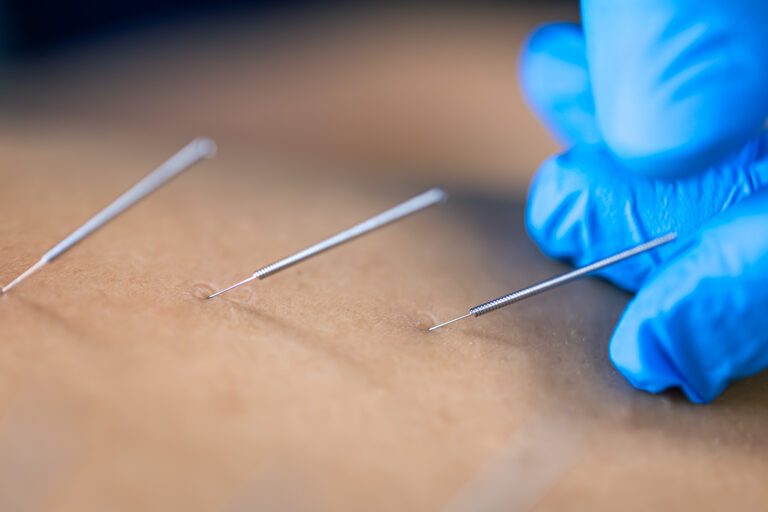
TREATMENT
- There are NO magic treatments for back pain that work for everybody unfortunately.
- It might not be one singular problem but a few different things happening together. A minor pain might be exacerbated by other things that are making you a bit more sensitive.
- Your therapist should be able to give you some basic advice or point you in the direction of others who can if it needs more specialist help.
- Lots of different treatments can help in the short term, such as a few hours or days, but don’t simply put your recovery in someone else’s hands. This has been shown to often be worse in the long term.
- You may have to avoid aggravating activities in the short term but make sure you go back to doing them. Nothing should be off limits in the long term. Don’t let anyone tell you otherwise.
- People who feel they need to protect their backs can also have worse outcomes.
- Learning more about what helps you and what makes you worse is important to help you manage your back pain. Your therapists should help you do this.
- Movement and exercise might help.
- Unfortunately here are no magic exercises for back pain. Find what you enjoy and just do it. This could be Pilates, strength training, sport with friends or simply going for a walk in the park.
- Don’t feel you have to really push yourself to get stronger or fitter but it is good once in awhile to exert yourself. This gets your body used to doing it.
- Moving and exercising can help us build confidence in our bodies and this might be key to recovery rather than fixing a physical problem.
PERSISTING BACK PAIN
- The common term for persisting pain is chronic pain, The term chronic does not mean ‘worse’ it is actually just a general term for pain that has gone on for longer than 3 months.
- How we respond to back pain might play a role in how long it lasts. If you change what you do in terms of activity such as avoiding things or think very negatively about your pain and your recovery.
- We could see persisting back pain as our protective systems, in this case pain, doing its job too well.
- Although pain is normal and a good thing, we could see it a lot like red wine. A little bit is great, but sometimes we can have too much of a good thing and it leaves us with a hangover.
- Persisting pain is currently seen as problem of the protective system itself rather than simply reflective of the state of your body.
- The more we work the mechanisms that contribute to pain the stronger they can get. It’s a bit like working your bicep in the gym. Just like your muscles the protective system can adapt and get better at protecting you.
- Unfortunately this means that the things that did not used to cause you pain now can do and may explain why you can be very sensitive to things that used to be normal.
- All of this does not mean you can’t get better but it is not as simple as finding an ‘off’ switch.
CLINICIANS ADVICE
This is some advice from some fantastic and experienced therapists from around the world who have kindly contributed to this document.
- Sheren Gaulbert – Stay connected with people who matter in your life/engage in activities you value.
- Karen Litzy – Don’t consider yourself broken or damaged goods.
- Ash James – Its often better to be at work than at home. You will move more, rest less and get back to normal stuff sooner.
- Kjartan Vibe Fersum – Important to have a shared plan (with your therapist) to move forward with.
- Tom Goom – It’s good to experiment with movement, relax into it and see what helps pain and stiffness. Movement is medicine, and like medicine it has a dosage, experimentation is needed to find the right dose for you.
- Claire Higgins – Your back is designed to be strong. It can so easily be visualised by patients to be a stack of blocks which could be “crushed” or “topple” at any moment. Education on how our backs are super strong and to trust in them is important.
- Claire Higgins – Focus on the things which turn your pain down, restoring balance e.g. exercise, meeting friends for coffee, being in the great outdoors.